prostatitisIs an inflammatory disease of the prostate. Manifested as frequent urination, pain in the penis, scrotum, and rectum, sexual dysfunction (erectile dysfunction, premature ejaculation, etc. ), sometimes urinary retention, and blood in the urine. The diagnosis of prostatitis is determined by urologists or andrologists based on typical clinical manifestations and results of rectal examination. In addition, ultrasound of the prostate, bakposev of prostate secretions and urine are performed. Conservative treatment - antibiotic therapy, immunotherapy, prostate massage, lifestyle modification.

General information
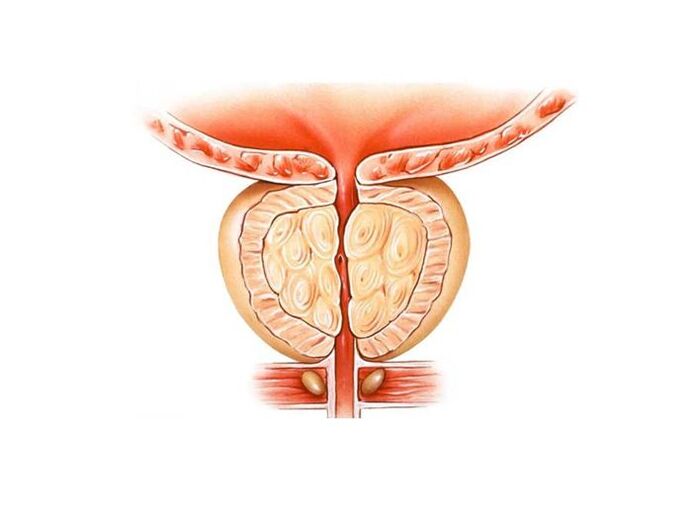
Prostatitis is inflammation of the seminal (prostatic) gland - the prostate gland. It is the most common disease of the male genitourinary system. Most commonly affects patients aged 25-50 years. According to various data, 30-85% of men over the age of 30 suffer from prostatitis. Abscesses may form in the prostate gland and inflammation of the testicles and appendages, threatening infertility. A rise in infection leads to inflammation of the upper genitourinary system (cystitis, pyelonephritis).
Pathology develops with the penetration of infectious agents, which enter the prostate tissue from urogenital organs (urethra, bladder) or from distant inflammatory foci (pneumonia, influenza, tonsillitis, furunculosis)
Causes of Prostatitis
As infectious agents in the acute process, Staphylococcus aureus, Enterococcus, Enterobacter, Pseudomonas, Proteus, Klebsiella) and Escherichia coli (E. Coli) can act. Most microorganisms belong to the conditional pathogenic group and can only cause prostatitis in the presence of other predisposing factors. Chronic inflammation is often due to multiple microbial associations.
The risk of developing this condition increases with hypothermia, a history of certain infections, and conditions that accompany congestion of prostate tissue. There are the following predisposing factors:
- General hypothermia (one-time or permanent, related to working conditions).
- A sedentary lifestyle, a profession that forces one to sit for long periods of time (computer operator, driver, etc. ).
- Frequent constipation.
- Violation of the normal rhythm of sexual activity (sexual hyperactivity, prolonged abstinence, incomplete ejaculation during "habitual" intercourse without emotional overtones).
- Presence of chronic diseases (cholecystitis, bronchitis) or foci of chronic infection (chronic osteomyelitis, untreated dental caries, tonsillitis, etc. ) in the body.
- Past urinary system diseases (urethritis, cystitis, etc. ) and sexually transmitted diseases (chlamydia, trichomoniasis, gonorrhea).
- Conditions that lead to suppression of the immune system (chronic stress, irregular and poor nutrition, frequent lack of sleep, overtraining in athletes).
It is hypothesized that chronic intoxication (alcohol, nicotine, morphine) increases the risk of developing pathology. Several studies in the field of modern andrology have demonstrated that chronic perineal trauma (vibration, concussion) in motorists, motorcyclists, and cyclists is a predisposing factor. However, the vast majority of experts believe that all these conditions are not the real cause of the disease, but only exacerbate the inflammatory process dormant in the prostate tissue.
Congestion of prostate tissue plays a decisive role in the occurrence of prostatitis. Violation of capillary blood flow leads to lipid peroxidation, edema, increased exudation of prostate tissue and creates conditions for the development of infectious processes.
Symptoms of prostatitis
acute prostatitis
Acute prostatitis is divided into three stages, which are characterized by certain clinical manifestations and morphological changes:
- acute catarrh. The patient complained of frequent urination, painful urination, sacral and perineal pain.
- acute follicle. The pain becomes more intense and sometimes radiates to the anus and is aggravated by bowel movements. Difficulty urinating with a thin stream of urine. In some cases, urinary retention occurs. A hypothermic state or moderate hyperthermia is typical.
- acute parenchyma. Severe systemic intoxication, hyperthermia to 38-40°C, chills. Urinary disorders, often - acute urinary retention. Sharp, throbbing pain in the perineum. Difficulty passing a bowel movement.
chronic prostatitis
In rare cases, chronic prostatitis becomes the result of an acute process, but often a primary chronic course is observed. Body temperature occasionally rises to low-grade fever. The patient noted mild pain in the perineum and discomfort during urination and defecation. The most typical symptom is the discharge of a small amount of fluid from the urethra during a bowel movement. The predominantly chronic form of the disease develops over a considerable period of time. It was preceded by prostatitis (blood stagnation in capillaries), which gradually turned into sterile prostatitis.
Chronic prostatitis is usually a complication of an inflammatory process caused by the pathogen of a specific infection (chlamydia, trichomonas, ureaplasma, gonorrhoeae). In many cases, the symptoms of a specific inflammatory process mask the manifestations of prostate damage. There may be slightly increased pain during urination, mild pain in the perineum, and a small amount of urethral discharge during defecation. Patients usually do not notice subtle changes in clinical presentation.
Chronic inflammation of the prostate can manifest as burning sensation in the urethra and perineum, dysuria, sexual dysfunction, and increased general fatigue. The consequences of violating potency (or the fear of those violating) often turn into mental depression, anxiety, and irritability. Clinical presentation does not always include all listed symptom groups, varies from patient to patient, and can change over time. Chronic prostatitis mainly has three characteristic syndromes: pain, dysuria, and sexual dysfunction.
There are no pain receptors in prostate tissue. Due to the rich innervation of the pelvic organs, inflammatory processes involved in the neural pathways, causes of pain in chronic prostatitis are almost inevitable. Patients complain of pain of varying intensities - from mild and aching to sharp and disrupting sleep. The nature of the pain changes (intensifies or decreases) with ejaculation, excessive sexual activity, or sexual abstinence. The pain radiates to the scrotum, sacrum, perineum, and sometimes to the waist.
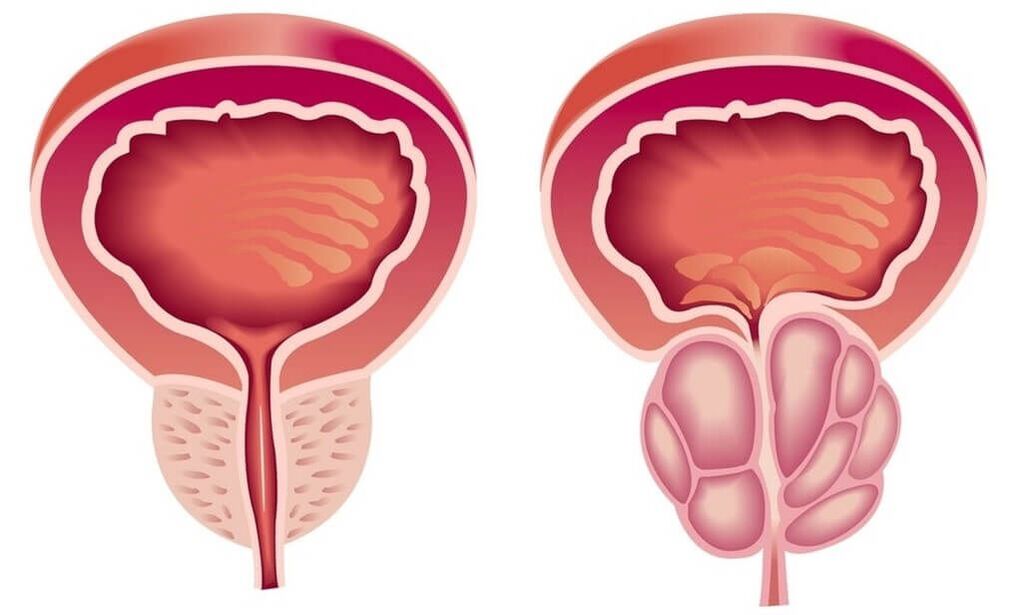
Due to the inflammation of chronic prostatitis, the volume of the prostate increases, squeezing the urethra. The lumen of the ureter narrows. The patient has frequent urination and a feeling of incomplete emptying of the bladder. Usually, dysuria manifests itself at an early stage. Compensatory hypertrophy then occurs in the muscle layers of the bladder and ureters. Symptoms of dysuria diminish during this period and then worsen again as adaptive mechanisms decompensate.
In the initial stages, dysfunction may occur, which manifests itself differently in different patients. Patients may complain of frequent nocturnal erections, blurred orgasms, or worsened erections. Accelerated ejaculation is associated with a reduction in the excitation threshold levels of the sexual pleasure centers. Pain during ejaculation can lead to denial of sexual activity. In the future, sexual dysfunction becomes more pronounced. In advanced stages, impotence develops.
The degree of sexual disturbance depends on many factors, including the patient's sexual constitution and psychoemotion. Violations of potency and dysuria may be due to changes in the prostate gland and to the patient's suggestion that if he suffers from chronic prostatitis, sexual and voiding disturbances are to be expected inevitably. Psychogenic dysfunction and dysuria are especially frequent in suggestible, anxious patients.
Impotence, and sometimes even the threat of sexual dysfunction, are intolerable for patients. There are often personality changes, irritability, disgust, excessive concern for one's own health, and even "taking care of illness".
complication
If acute prostatitis is not treated promptly, there is a significant risk of developing a prostate abscess. As purulent lesions develop, the patient's temperature rises to 39-40°C and becomes tense. Hot periods alternate with severe cold. Severe pain in the perineum makes it difficult to urinate and prevent bowel movements.
Increased prostatic edema leads to acute urinary retention. Rarely, an abscess ruptures spontaneously into the urethra or rectum. When it is opened, purulent, cloudy urine appears in the urethra with an unpleasant irritating odor; when it is opened, the feces in the rectum contain pus and mucus.
Chronic prostatitis is characterized by a fluctuating course with long periods of remission, during which the inflammation in the prostate is dormant or manifests poor symptoms. Patients who are not bothered by anything usually stop treatment and only turn around when complications arise.
Transmission of infection through the urinary tract causes pyelonephritis and cystitis to occur. The most common complications of the chronic process are inflammation of the testicles and epididymis (epididymo-orchitis) and inflammation of the seminal vesicles (vesiculitis). The result of these disorders is often infertility.
diagnosis
Typical clinical presentation simplifies the diagnostic process of acute and chronic prostatitis. must:
Prostatitis Treatment
Treatment of acute prostatitis
Patients with uncomplicated acute processes were treated by urologists on an outpatient basis. In case of severe poisoning, a suppurative process is suspected, hospitalization is required. Get antimicrobial therapy. Preparations are chosen taking into account the susceptibility to infectious agents. Widely used antibiotics penetrate very well into prostate tissue.
With the development of acute urinary retention on the background of prostatitis, they resort to installing a cystostomy instead of a urinary catheter because of the risk of forming a prostatic abscess. As the abscess develops, endoscopic transrectal or transurethral incision of the abscess is performed.
Treatment of Chronic Prostatitis
Treatment of chronic prostatitis should be complex, including symptomatic therapy, physical therapy, immunocorrection:
- antibiotic treatment. The patient was prescribed a long course of antibiotics (within 4-8 weeks). The choice of the type and dose of antibacterial drugs, as well as the determination of the duration of the course of treatment are carried out individually. According to the results of urine culture and prostatic secretion, the drug is selected according to the sensitivity of the microflora.
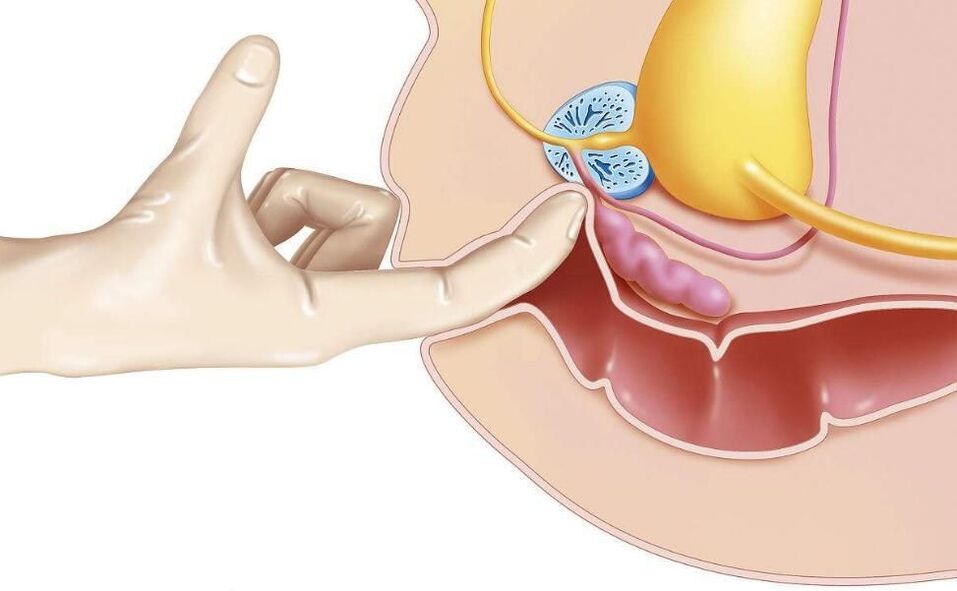
- Prostate massage.Massaging the glands has complex effects on the affected organs. During the massage, the inflammatory secretions accumulated in the prostate are squeezed into the duct, then into the urethra and out of the body. The procedure improves blood circulation to the prostate, which minimizes congestion and ensures better penetration of antibacterial drugs into the tissue of the affected organ.
- physiotherapy.To improve blood circulation, laser irradiation, ultrasonic waves, and electromagnetic vibrations are used. If a physical therapy procedure is not possible, the patient is prescribed warm medicinal microcapsules.
In chronic, long-standing inflammation, consultation with an immunologist is recommended to select strategies for immunocorrective therapy. Advise patients on lifestyle changes. Making certain changes in the lifestyle of patients with chronic prostatitis is not only a treatment measure, but also a preventive measure. Advise patients to normalize sleep and wakefulness, establish dietary habits, and engage in moderate physical activity.
Antibiotic therapy is most effective in the treatment of prostatitis. Phytotherapy, immune correctors and hormonal preparations are also available upon doctor's prescription.
In the absence of acute symptoms, prostatitis can be treated with physical therapy. In case of abscesses and suppuration, surgical intervention is recommended.
medical treatement
Treatment of prostatitis by antibiotic therapy should start with bakposev, the purpose of which is to assess the sensitivity of the body to such antibiotics. Violation of urination, a good result is the use of anti-inflammatory drugs.
In acute cases, the drug is given in tablet form - in the form of a dropper or intramuscular injection. For the treatment of chronic forms of prostatitis, rectal suppositories are effective: with their help, the drug reaches its target faster and with minimal impact on other organs.
Blood thinners and anti-inflammatory drugs have also proven their effectiveness.
antibacterial therapy
Antibiotics are effective drugs against bacterial prostatitis. In order to achieve the desired effect without harming the body, the choice, dosage and treatment plan of the drug should be handled by the doctor. In order to correctly choose the most effective drug, he had to find out the type of pathogen causing prostatitis and check the patient's tolerance to a specific group of antibiotics.
For the effective treatment of chronic prostatitis, fluoroquinolone antibiotics have proven their effectiveness. Their action is aimed at inhibiting bacterial infections and enhancing the body's own immunity. In addition, bacteriostatic antibiotics are recommended for the prevention and treatment of concomitant diseases of the genitourinary system.
For the treatment of prostatitis caused by mycoplasma and chlamydia, macrolides and tetracyclines can be added to slow down the spread of infection.
Antibiotics are taken for 2 to 4 weeks. In cases of positive dynamics, the course can be extended.
physiotherapy
Physiotherapy methods for the treatment of prostatitis are aimed at activating blood circulation in the pelvic area, improving metabolic processes in the prostate, and cleaning the ducts. The effect of the latter is enhanced if physical therapy is combined with taking antibiotics.
The main methods include:
- magnetic therapy;
- Laser Treatment;
- Electrophoresis;
- warm up;
- ultrasound;
- mud treatment;
- High frequency irradiation;
- physiotherapy.
According to modern research, one of the oldest methods - transrectal prostate massage has not yet proven its effectiveness.
non-specific treatment
Nonspecific treatments for prostatitis include:
- leech therapy;
- therapeutic fasting;
- acupuncture;
- Diet according to the method of Ostrovsky;
- Alkaline the body according to the method of Neumyvakin.
It is highly recommended to coordinate all non-traditional methods of treating prostatitis with your doctor.
Operation
Surgical approach in complicated and urgent situations:
- For the drainage of purulent abscesses, which are removed laparoscopically by puncture;
- Violation of urination due to damage to the urinary tract;
- The affected area is large;
- There are a lot of stones in the gland.
Stones and hardened tissue are removed endoscopically. If there is extensive damage or multiple stones, the prostate needs to be removed.
Transurethral resection is also effective for bacterial prostatitis. Therefore, the risk of recurrence can be reduced.
folk remedies
Folk remedies for prostatitis alone are unlikely to be effective, but they may be useful in combination with medical and physical therapy methods. These include: beekeeping products, herbal and seed decoctions, garlic tincture, ginger, castor dew, fresh vegetables, pumpkin seeds.
In acute cases of the disease process, you must consult a doctor, and in no case should you self-medicate! If a purulent abscess ruptures, it can be fatal.
prostatitis candle
Rectal suppositories are more effective than pills for treating prostatitis because the rectum is closer to the prostate, which means the medicine will work faster.
The composition of drugs for the treatment of prostatitis can be quite different, they are prescribed to solve specific problems.
- Antimicrobials are especially effective against prostatitis caused by chlamydia.
- Painkillers are used in symptomatic treatment and provide good pain relief.
- Immunostimulants improve circulation, relieve swelling, and are used in complex treatments.
- Herbal preparations are mild in action. They are used like candles on bee products and are used as a supplement to main treatments.
- Compositions based on fish phenols promote blood flow in the area of the intestinal mucosa, which accelerates the weakening of inflammatory processes and slightly increases immunity.
- Enzyme-based products prevent the formation of scar tissue. It is recommended as part of a combination of antibiotics, anti-inflammatory and analgesic medications.
Auxiliary drugs
For the symptomatic treatment of male prostatitis, such as the relief of pain during urination, antispasmodics can be added to relax the smooth muscle, thereby quickly relieving the pain.
Blood-thinning and anti-inflammatory dietary supplement based on bee products, pumpkin seed oil, palm fruit extract to aid overall recovery.
Diet and Lifestyle
For the treatment of prostatitis, a correct, balanced diet and a healthy lifestyle are very important. Food should not contain spicy, fried, salty, pickled food. In acute form, alcohol consumption is strictly prohibited.
Food should contain enough fiber to prevent constipation. Protein content should be reduced. It is best to supplement the diet with herbs, ginger, pumpkin seeds.
non-drug treatment
Non-drug treatments allow you to act directly on the prostate, increasing the concentration of the drug in its tissue and helping to decongest it.
Microwave heat therapy is administered using a rectal probe inserted into the patient's anus. On the device, you can set the desired temperature for a particular type of exposure. To increase drug concentration in the prostate, heating to 38-40°C is required. For antibacterial effect - 40-45 ° C.
Today, non-drug treatments focus on laser therapy. The possibilities of this technique are extensive. Under the influence of laser light, the following processes occur in the prostate gland:
- Activation of redox reactions;
- Improve blood microcirculation;
- formation of new capillaries;
- The pathogenic flora is suppressed;
- The process of cell division is activated, which helps in tissue regeneration.
During the study of the effect of laser treatment on prostatitis patients, a side effect was noticed, but positive for therapeutic purposes. Among those who completed the course, potency increased, erectile dysfunction was eliminated, and vitality was restored. To achieve this result, it is necessary to use beams with specific wavelengths. Generally, low-level laser radiation is used to treat chronic prostatitis.
Patients can voluntarily receive laser treatment if the attending physician does not prescribe it.
Surgical Treatment of Chronic Prostatitis
Chronic prostatitis will not pose a threat to the patient's life, but will significantly reduce its quality. The most serious complication of this disease is the formation of stones in the glandular tissue. To free it from the prostatic stones, transurethral resection is used.
The surgery was performed under the control of TRUS.
If complications such as prostatic sclerosis develop, transurethral electrosurgery is performed. If, in combination with this pathology, sclerosis of the bladder neck is observed, partial resection of the prostate is performed.
With occlusion of the vas deferens and excretory ducts, endoscopic surgery is indicated to remove the violation of secret patency. For this, an incision is made in the seminal vesicle and excretory duct. For abscesses, complete removal of the gland is possible.
Consequences of untreated prostatitis
Even if the symptoms of prostatitis have not appeared for a long time, it is necessary to undergo regular examinations by a urologist. Incompletely cured prostatitis may be accompanied by the formation of calcifications, which must then be removed together with the gland. Experts are sure there is no other way to remove or dissolve the stones.
In addition, pathogenic microorganisms can migrate to adjacent organs, causing inflammation. Running prostatitis can lead to the development of adenomas and prostate cancer.
Prediction and Prevention
Acute prostatitis is a disease with obvious chronic tendency. Even with timely and adequate treatment, more than half of the patients eventually develop chronic prostatitis. Recovery is far from always possible, however, with correct and consistent treatment and following your doctor's recommendations, it is possible to eliminate unpleasant symptoms and achieve long-term stable remission during chronic processes.
Prevention is the elimination of risk factors. It is necessary to avoid hypothermia, alternate between sedentary work and physical activity, eat regularly and adequately. For constipation, laxatives should be used. One of the preventive measures is the normalization of sexual life, since both excessive sexual activity and sexual abstinence are risk factors for the development of prostatitis. If you develop symptoms of urinary tract or sexually transmitted diseases, you should seek medical attention promptly.





























