What is prostatitis
Types and first signs of illness
- acute bacterial prostatitis: Caused by a bacterial infection that usually comes on suddenly and may resemble flu-like symptoms. This is the least common of the four types of prostatitis.
- chronic bacterial prostatitis: Characterized by recurrent bacterial infections of the prostate. There may be few symptoms between attacks, which is why it can be difficult to treat successfully.
- Chronic prostatitis/chronic pelvic pain syndrome: Most cases of prostatitis fall into this category, but at the same time this type is the least understood. It can be classified as inflammatory or non-inflammatory, depending on the presence of infection-fighting cells (antibodies in urine, semen, and prostate secretions). It is often impossible to identify a single specific cause. Symptoms may come and go or appear intermittently.
- asymptomatic inflammatory prostatitis: This disease is often diagnosed incidentally during treatment for infertility or prostate cancer. People with this form of prostatitis have no symptoms or symptoms of discomfort, but tests show the presence of infected cells in the prostate secretions.
The main symptoms
- Pain or burning when urinating (dysuria);
- Difficulty urinating, such as thin urine or urinary stasis, intermittent urination;
- Frequent urination, especially at night (nocturia - going to the bathroom more than twice a night);
- Urgent need to urinate.
- In the rectum (rectum), sometimes accompanied by constipation;
- in the abdomen and/or lower back;
- In the perineum - between the scrotum and the rectum.
- Fever and chills;
- general malaise and body aches;
- swollen lymph nodes;
- Sore throat.
- Cloudy urine or blood in the urine;
- discharge from urethra;
- Urine and secretions have an unpleasant odor.
diagnosis method
lab testing
- clinical blood and urinalysis;
- Bacterioscopy and culture of urine sediment and prostate secretions – samples are examined under a microscope for the presence of bacteria;
- Smear of urethral discharge (if discharge is present);
- Prostate-specific antigen (PSA) levels are measured.
PSA levels may also be slightly elevated due to benign enlargements of the prostate (adenomas) and urinary tract infections.
Age-Related PSA Indicators - Table
| generation | PSA standard |
|---|---|
| Under 40 years old | Less than 2. 5 ng/ml |
| 40-49 years old | 2. 5 ng/ml |
| 50-59 years old | 3. 5 ng/ml |
| 60-69 years old | 4. 5 ng/ml |
| Over 70 years old | 6. 5 ng/ml |
Musical instrument studies
- Bladder Urodynamic Study- Complex instrumental methods using special equipment allow you to determine whether the bladder is completely empty, urine flow, pressure within the bladder and urethra, and to evaluate the impact of prostatitis on normal urination. This study is recommended for people with chronic urinary problems: intermittent or trickling flow, incontinence, frequent urination, etc. It is also indicated for patients with long-term inflammation of the prostate, especially when standard treatments are ineffective. Before the examination, a special catheter sensor, which is also connected to a measuring device, is inserted into the patient's urethra in a horizontal position. Next, let the patient drink a certain amount of clean water, and at the same time record the feeling of bladder fullness, the urge to urinate for the first time, whether there is urine leakage, etc. The patient is then transferred to a specially equipped chair and seated in the chair. He needs to be relieved under the control of sensors and equipment that make the necessary measurements. The process consists of several stages, each taking approximately half an hour. The results of the urodynamic study are provided to the patient immediately upon completion.
- Ultrasound Imaging (USA)- This method is used to diagnose existing diseases and is also suitable for men after the age of 45 for the annual prevention of prostatitis and other glandular diseases. The study was performed using an ultrasound machine through the anterior abdominal wall in the morning on an empty stomach, with the bladder filled with clean water, and a special transducer inserted 5-7 cm deep into the rectum (rectal method) or through the urethra. This procedure is completely safe and allows you to determine the contour, size and condition of various areas of your prostate. The volume of a healthy prostate is approximately 20-25 cm3. The maximum length, width and thickness are 3. 5 cm, 4 cm and 2 cm respectively.
- Magnetic resonance imaging (MRI)- This method allows you to study the structure, density, condition and even blood flow of the prostate in detail; sometimes, additional contrast material is injected intravenously to better understand the situation. This test can also be used to differentiate between prostatitis and tumors. The MRI machine is a large cylinder surrounded by magnets into which the medical table carrying the patient slides, like a tunnel. For 10-12 hours before surgery, patients should wear loose-fitting clothing (without hardware) and avoid eating large amounts of food. Watches, jewelry and any other metal objects must be removed before the inspection. MRI diagnostic methods are contraindicated if the patient has metal-containing implants or cardiac devices. To perform this procedure, a transrectal sensor is most often used (although it is also possible without it), having previously cleaned the rectum with an enema. The nurse inserts the sensor and secures it with a special disposable cuff. The patient should lie as still as possible throughout the examination (approximately 30 minutes). The procedure is painless.
- Cystoscopy- A cystoscope is used to examine the mucous membrane of the urethra and bladder - A long, narrow catheter with a light bulb and a camera at the end is used under local anesthesia. This surgery is performed after the bladder is full. The duration of a cystoscopy is approximately 15 minutes. This method allows you to evaluate the condition of your urinary tract and rule out other conditions that may be causing urinary problems.
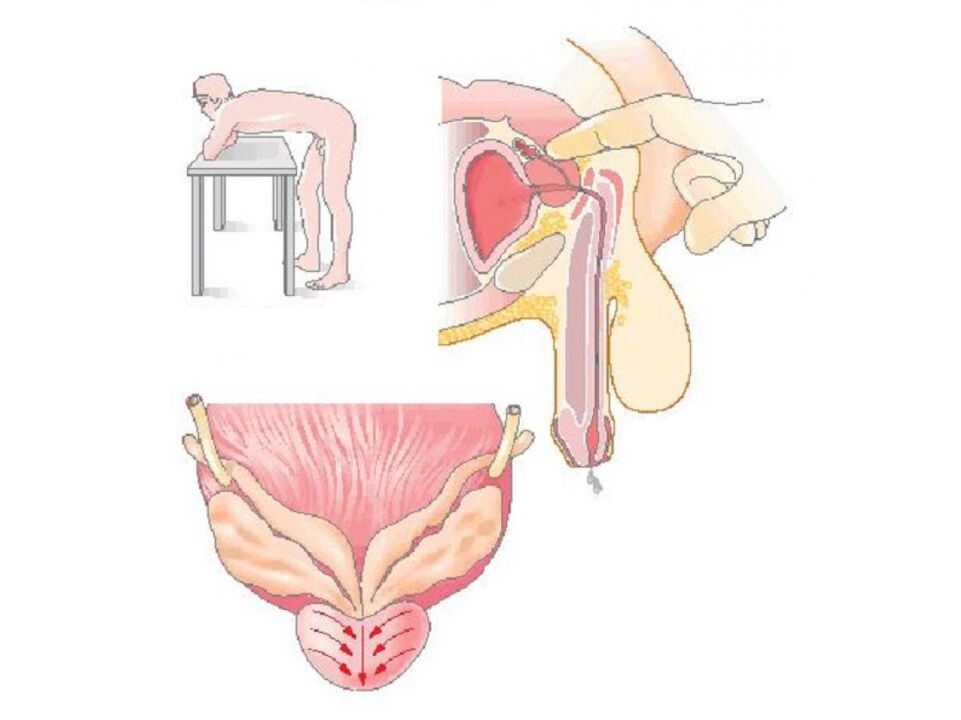
- prostate biopsy- This is a necessary procedure if, after a thorough examination, the doctor suspects a malignant process in the prostate. Must be ruled out or confirmed before a treatment strategy can be selected. The procedure is performed on an outpatient basis, in which a needle is inserted into the patient's rectum and a sample of prostate tissue is collected. A local anesthetic is injected into the anus, and then, once the anesthetic has taken effect, an ultrasound probe with a needle attachment is inserted into the intestine. Under ultrasound guidance, the surgeon determines where the material needs to be "pinched off" for analysis. Typically, there are up to 18 different points on the organ. The biopsy will not cause pain; there may be only mild discomfort after the anesthesia wears off.

%20and%20inflamed%20(right)%20prostate%20on%20MRI%20image.jpg)
Differential diagnosis
Doctors say inflammation of the prostate does not increase the risk of prostate cancer.





























